There were about 15 of us swimming in the freshwater pools at WorldSprings, a mineral hot spring spa in Dallas, Texas. Ostensibly, we’re here to enjoy a floating sound bath, but throughout the meditation experience, our eyes remain focused on Dr. Sarah Gottfried. Even in a swimsuit and sunglasses, you can feel the majesty of the fourth new york times Bestselling author. The board-certified physician, a graduate of Harvard and MIT, is heading to Destination Dallas (where she serves as a wellness consultant for WorldSprings) for a sound bath, guiding us through anti-inflammatory circuits of saunas, cold baths, and hot baths . most us All around her.
Featured image by Riley Blanks Reed.

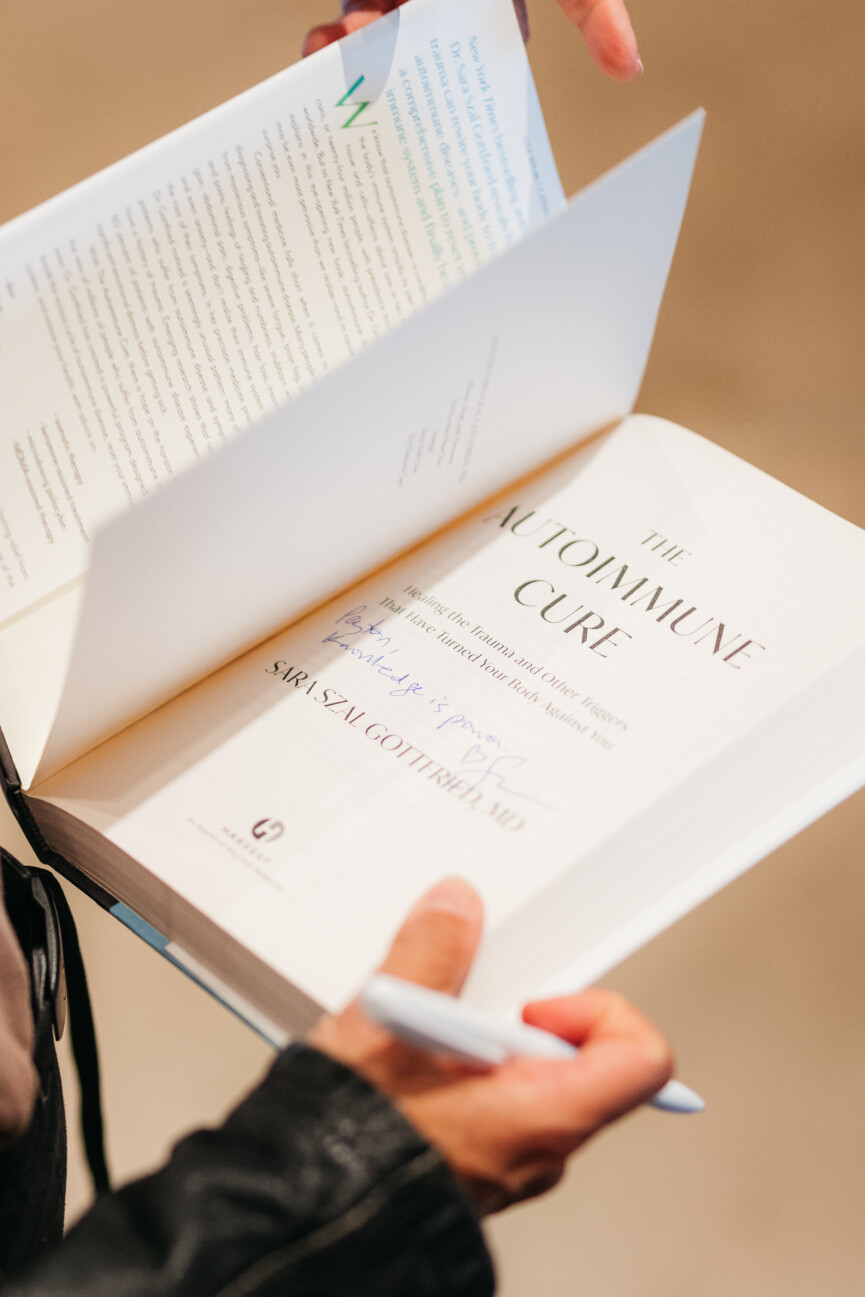
Autoimmune disease and trauma: A conversation about this surprising connection
As soon as the sound bath ended, the fan girls started. “Your work has changed my life” is a resounding exclamation. Dr. Gottfried’s book covers everything from hormonal detoxification to slowing the aging process, all while taking control of your health—especially as a woman. “Don’t give your power to your doctor or nurse,” Dr. Gottfried shared with me. “No one knows your body like you do.”
“Don’t hand over your authority to your doctor or nurse practitioner. No one knows your body like you do. – Dr. Sara Gottfried
Dr. Gottfried’s latest book focuses researchers’ attention on autoimmune diseases, which have increased dramatically in recent years, especially in women. She came up with a surprising reason.
“I’ve seen a huge uptick in autoimmunity in my practice during the pandemic, and increased trauma seems to be at the root of it,” Dr. Gottfried shared. “I listen to what my patients tell me, and this is something I’ve seen from my practice. The narrative from hundreds of patients: more trauma and more autoimmunity.”
After a series of saunas, cold baths, and global-style soaks, I spoke with Dr. Gottfried to learn more about her latest work. The renowned doctor shares her thoughts on Adverse Childhood Experiences (ACEs), psychedelic treatment, and the supplements most women may need to take.

Sara Gottfried, Ph.D.
Dr. Sara Gottfried is a four-time winner of the New York Times Best-Selling Author Award for Innovative Integrative Health. She is a Harvard and MIT-educated physician, speaker, yoga teacher, and author. She is a clinical assistant professor in the Department of Integrative Medicine and Nutritional Sciences at Thomas Jefferson University and director of precision medicine at the Marcus Institute for Integrative Medicine.
What first led you to investigate trauma as a trigger for autoimmune disease?
The three necessary conditions for developing an autoimmune disease are genetic predisposition, leaky gut, and triggers. Triggers can be general hormonal changes, such as postpartum, perimenopause or menopause. It could also be an infection, like COVID-19, or a traumatic experience. It can be loneliness or isolation. I’ve seen a huge spike in autoimmunity in my practice during the pandemic, and increased trauma seems to be at the root of it.
Are there any particular traumas that predispose to autoimmune diseases?
The most studied type of trauma is adverse childhood experiences (ACEs), or exposure to abuse, neglect, or other difficulties during childhood. You can find out your ACE score here.
Autoimmune diseases disproportionately affect women. Why do you think this is?
According to the ACE study, women experience approximately 10% more trauma than men. We also have more significant hormonal changes during pregnancy, postpartum, perimenopause and menopause. Hormones regulate the immune system. These are gender differences. There are also socially created gender disparities that may deprive women of their health and increase their risk of autoimmunity, such as higher demands on caregivers and lower wages for equal work. All of these factors put women at greater risk of developing autoimmune diseases, so four out of five people with autoimmune diseases are women.
I enjoyed your discussion with Dr. Mark Hyman about the different types of psychedelic therapy. How do you think they differ from traditional talk therapy when it comes to treating trauma?
Psychedelic-assisted therapy, unlike traditional talk therapy, appears to be more effective in addressing post-traumatic stress disorder. Talk therapy is about 30% effective in resolving PTSD. One form of psychedelic therapy, MDMA-assisted therapy, is 67 to 71 percent effective, so it’s more than twice as effective. Psychedelic-assisted therapy has been shown to be helpful in preliminary studies for a variety of conditions, including treatment-resistant depression, hospice care, and eating disorders.
What would you say to someone who has never tried psychedelic therapy? How have they helped you in your own healing journey?
Although many traditional psychedelics have been used for thousands of years, we are still in the early stages of understanding the benefits of psychedelic therapy. When it comes to whether to consider psychedelic treatment, it’s important to know that, despite the “just say no” anti-drug movement, psychedelics are safer than alcohol. There are other ways to achieve healing states of consciousness, such as Holotropic Breathing, as I describe in “Autoimmune Therapy.”
In my experience, psychedelic-assisted therapy is an accelerator in the trauma healing process.
Can you explain the pine system and how trauma relates to it?
Trauma may remain in the body, specifically in the psychoimmune neuroendocrine system, or PINE system. The PINE system describes your reaction to your environment. This concept is sometimes described as psycho-neuro-endocrine-immunology. I prefer PINE because it’s easier to remember. PINE is a field of scientific research that studies two-way communication between the brain and its functions, the immune system, the nervous system, the endocrine system, and how they relate to physical, mental and spiritual health. You can think of PINE as your stress response system. Some of us have very sensitive PINE systems; others have very sensitive PINE systems. Others don’t.
What are some of your favorite wearables that track heart rate variability?
The wearables I’ve found most helpful with HRV are the Oura Ring and Eight sleep, a system that mounts to the mattress, tracks and optimizes sleep, and has helped me improve my HRV more than any other device.
Are there any supplements you would recommend to all women?
I don’t recommend a blanket magnesium supplement for everyone, but the most common supplement women need is magnesium, especially if you suffer from chronic tension. About 75 to 80 percent of us are nutritionally deficient. I usually recommend starting with 150 to 300 mg in the evening.
Your new book empowers those who want to take control of their health. What information or advice do you hope people take away from your book?
Do not give your authority to your doctor or nurse practitioner. No one knows your body like you do, so empowerment includes testing your own autoimmunity to see if you’re one of the 30% of Americans who do.

